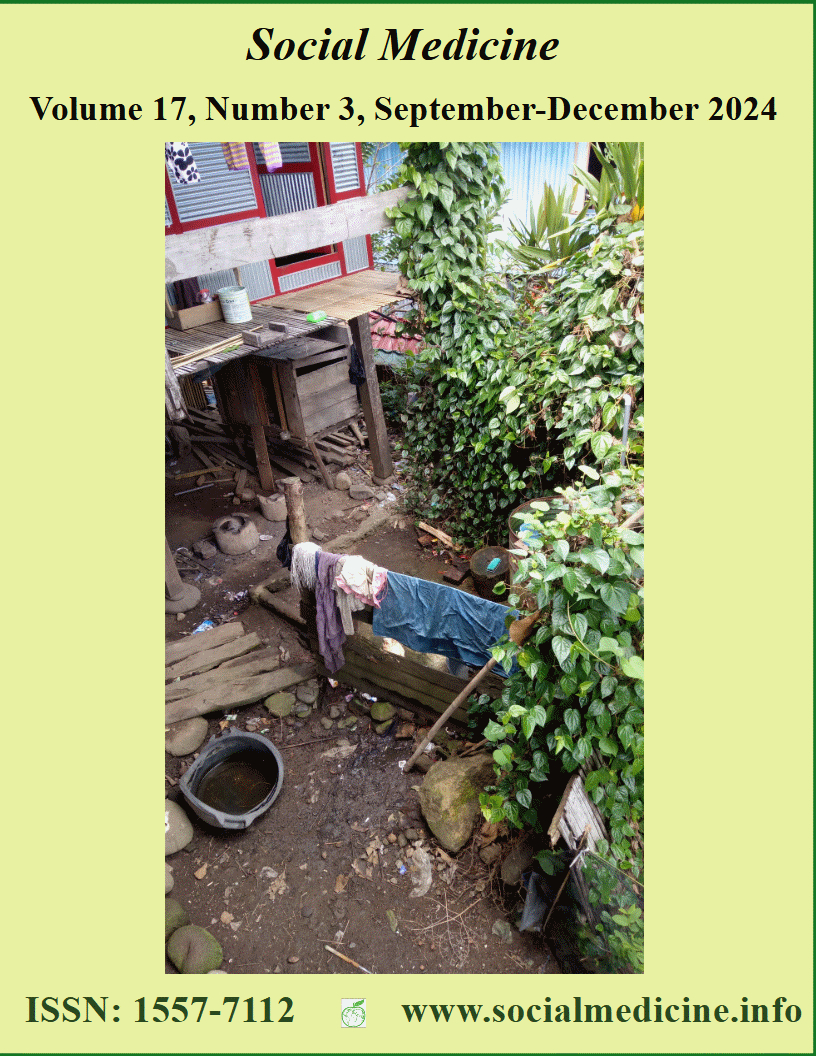
An Occupational Health Perspective of Nurses’ Quality of Life in Indonesia
Abstract
This study aims to develop factors and indicators of aspects that shape nurses' quality of life. It was conducted using a cross-sectional design, while the population consisted of nurses working in the inpatient ward totaling 915. The sample size was determined by the rule of thumb criteria which produced 270 nurses. The samples were selected using the simple random sampling technique, while data was collected with a questionnaire that had been tested for its validity and reliability. The endogenous variable hypothesis test was carried out by SEM-PLS analysis. The results showed that health aspects affect nurses' quality of life, as physical health sharpens engagement in professional activities and social relationships. Spiritual influence on nurses' quality of life, as well as the ability to withstand stress, anxiety, and depression, depend on the value of trust in God. Furthermore, the workplace standard affects the quality of life, while job satisfaction influences the achievement of welfare. The work environment is the main stressor for workers about job satisfaction and self-actualization. The Indonesian government needs to formulate policies to support work environment management in health service agencies, as well as facilitate the Indonesian Nurses Association to improve nurses' quality of life and increase their competence.
References
Kosim N, Istiyani N, Komariyah S. Post traumatic stress disorder pada pasien kecelakaan lalu lintas. Artik Ilm Mhs. 2015;1(1):1-7.
Santos JMP dos, Oliveira SB De. A Financial Theory Perspective of the Metrics Employed to Measure Value in the “value in Healthcare” Methodologies. Port J Public Heal. 2021;38(3):176-186. doi:10.1159/000512564
Khatib AH, Hamdan-Mansour AM, Bani Hani MA. Theoretical Perspectives of Hospitalized Older Patients and Their Health-Related Problems and Quality of Care: Systematic Literature Review. Open Public Health J. 2017;10(1):215-225. doi:10.2174/1874944501710010215
An J-G, Gao X-M, Ma Y-X, Xiao S-X. Relation between depression, anxiety, and quality of life among female nurses in Shaanxi province: a cross-sectional study. Lancet. 2015;386:S29. doi:10.1016/s0140-6736(15)00610-8
WHO. Social Determinants of Health and Well-Being among Young People. Vol 30.; 2012. http://www.euro.who.int/pubrequest
Sirin M, Sokmen MS. Quality of Nursing Work Life Scale: The psychometric evaluation of the Turkish Version. Int J Caring Sci. 2015;8(3):543-554. doi:http://dx.doi.org/10.1016/0091-6749(85)90054-5
Morsy S, Sabra H. Relation Between Quality of Work Life and Nurses Job Satisfactionatassiut University Hospitals. Al-Azhar Assiut Med J. 2015;13(1).
Utami TN. Tinjauan Literatur Mekanisme Zikir Terhadap Kesehatan: Respons Imunitas. J JUMANTIK. 2017;100 (1).
Santosa H, Mutiara E, Hasan W, Sudaryati E. Confirmatory Factor Analysis of Work-Life Quality for Female Nurses in Medan City , Indonesia. 2021;8(5):3828-3833.
Wijayatno S. Structural Equation Modeling Dengan Lisrel 8.8. Graha Ilmu; 2009.
Sholihin M, Ratmono. Analisis SEM-PLS Dengan WarpPLS 3.0. ANDI; 2013.
WHO. WHOQOL: Measuring Quality of Life. Published online 2018. https://www.who.int/tools/whoqol
Jacob DE, Sandjaya. Faktor faktor yang mempengaruhi kualitas hidup masyarakat Karubaga district sub district Tolikara propinsi Papua. J Nas Ilmu Kesehat. 2018;1(69):1-16.
Diana, Eliyana A, Mukhtadi, Emur AP. Quality of Work Life and Nurse Performance: The Mediation of Job Satisfaction in Pandemic Era. Syst Rev Pharm. 2020;11(11):1739-1745. doi:10.31838/srp.2020.11.243
Wu XY, Zhuang LH, Li W, et al. The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: a systematic review and meta-analysis. Qual Life Res. 2019;28(8):1989-2015. doi:10.1007/s11136-019-02162-4
Hafizh MA, Luh N, Hariastuti P. Pengaruh Quality of Work Life dan Burnout terhadap Kinerja Karyawan Melalui Kepuasan Kerja Sebagai Variabel Moderasi (Studi Kasus : CV. XYZ). Pros SENASTITAN Semin Nas Teknol Ind Berkelanjutan. 2021;1(1):89. https://ejurnal.itats.ac.id/senastitan/article/view/1653
Utami TN, Nurhayati, Harahap R., Aidha Z. Reproductive Health of Women Workers in Villages, Cities in Islamic Perspective. Heal Notions. 2020;4(4):123-128. doi:http://dx.doi.org/10.33846/hn40404
Khani S. Psycho-social experience of oocyte recipient women: a qualitative study. BMC Womens Health. 2021;21:1-8.
Riba M. Distress Management. HHS Public Access. 2019;17(10):1229-1249.
Viake J. Psychologic Distress and Quality of Life After ICU Treatment for Coronavorus Disease 2019: A Multicenter, Observational Cohort Study. Crit Care Explor. Published online 2021:1-2.
Hansen L. Physical and Mental Quality of Life in Patients with End-Stage Liver Disease and Their Informal Caregivers. HHS Public Assess. 2020;19 (1):155-161.
Amin M, Efendy I, Utami TN. Analysis of Factors that Influence Nurse’s Work Stress at the Inpatient Room of General Hospital Regional Doctor Zubir Mahmud Regency of East Aceh. J La Medihealtico. 2022;3(5):392-409. doi:10.37899/journallamedihealtico.v3i5.707
Bliss MM, Krzystowczyk J. Inclusive and Gender: Protecting Workers’ Reproductive Health. Prof Saf. 2018;63(03):38-43. www.asse.org
Khademian Z, Ara FK, Gholamzadeh S. The effect of self care education based on Orem ’ s nursing theory on quality of life and self-efficacy in patients with hypertension. Int J Community Based Nurs Midwifery. 2019;8(2):140-149. doi:10.30476/IJCBNM.2020.81690.0.140
Alıcı CB, Koç Z. Quality of life and satisfaction affect individualized nursing care perceptions in intensive care. Psychol Heal Med. 2020;25(2):148-159. doi:10.1080/13548506.2019.1654110
Yang HM, Kim HR. Differences in health and related factors among older working women, according to productive engagement types. Soc Med. 2024;17(1):20-28.
Putri DE. Hubungan fungsi kognitif dengan kualitas hidup lansia. JIP, J Ilmu Penelit. 2021;2(4):1147-1152.
Lucaccioni H, Costa C, Duque MP, Balasegaram S, Sá MacHado R. Risk of COVID-19 in Health Professionals: A Case-Control Study, Portugal. Port J Public Heal. 2021;39(3):137-144. doi:10.1159/000519472
Raes S, Vandepitte S, De Smedt D, Wynendaele H, DeJonghe Y, Trybou J. The relationship of nursing home price and quality of life. BMC Health Serv Res. 2020;20(1):1-10. doi:10.1186/s12913-020-05833-y
Jones S, White S, Ormrod J, et al. Work-based risk factors and quality of life in health care workers providing maternal and newborn care during the Sierra Leone Ebola epidemic: Findings using the WHOQOL-BREF and HSE Management Standards Tool. BMJ Open. 2020;10(11):1-10. doi:10.1136/bmjopen-2019-032929
Fumincelli L, Mazzo A, Martins JCA, Mendes IAC. Quality of life and ethics: A concept analysis. Nurs Ethics. 2019;26(1):61-70. doi:10.1177/0969733016689815
Amin M, Efendy I, Utami TN. Analysis of Factors that Influence Nurse's Work Stress at the Inpatient Room of General Hospital Regional Doctor Zubir Mahmud Regency of East Aceh. Journal La Medihealtico. 2022. 03 (05): 392-409. doi: 1037899/journallamedihealtico.v3i5.707.
Ruiz-Fernandez M, Perez-Garcia E, Ortega-Galan AM. Quality of Life in Nursing Professionals:Burnout, Fatique, and Compassion Satisfaction. Int. J. Environ. Res. Public Health. 2020, 17, 1253; doi:10.3390/ijerph17041253.
Orszulak N, Kubiak K, Kowal A, Czapla M, Uchmanowicz I. Nurses’ Quality of Life and Healthy Behaviors. Int. J. Environ. Res. Public Health. 2022, 19, 12927. doi: doi.org/10.3390/ijerph191912927.
Yang HM, Kim HR. Differences in health and related factors among older working women, according to productive engagement types. Social Medicine. 2024. 16 (1). 20-28
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Social Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.