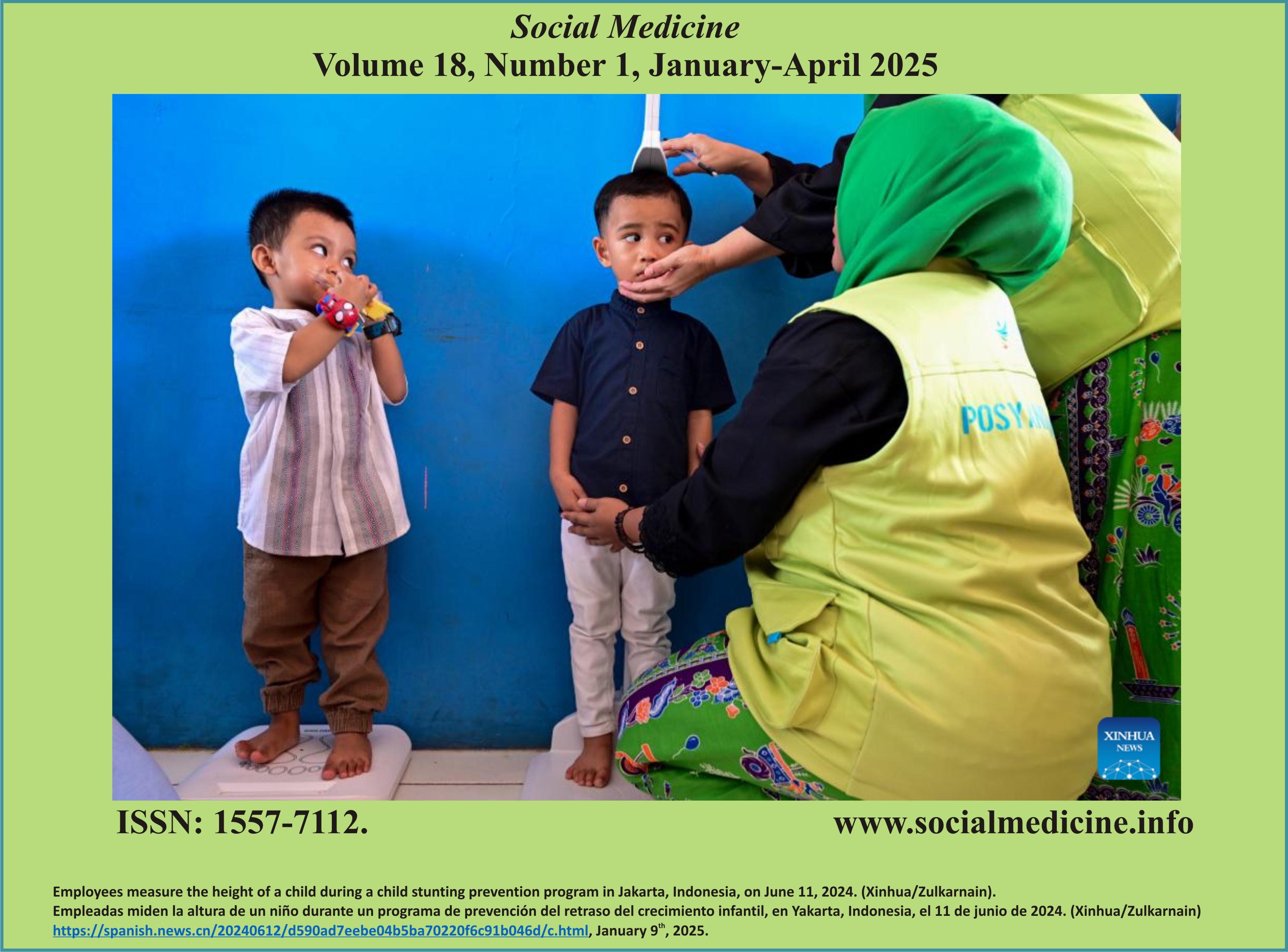
Socioeconomic Disparities in Maternal Health Facility Utilization at Hospital: Evidence from Indonesia's 2018 Basic Health Research
DOI:
https://doi.org/10.71164/socialmedicine.v18i01.2025.1763Abstract
Maternal and neonatal mortality remain critical issues, especially in developing countries like Indonesia. This study aims to analyze socioeconomic disparities in hospital utilization for childbirth in Indonesia using data from the 2018 Indonesian Basic Health Research. The study found that socioeconomic factors significantly influence hospital utilization by pregnant women, with higher socioeconomic status associated with higher hospital utilization. Urban residence, higher education level, employment status, and health insurance ownership positively correlated with hospital utilization. These findings highlight the need for targeted interventions to improve access and utilization of maternal health facilities, particularly among vulnerable socioeconomic groups. The study contributes to the literature by providing new insights into socioeconomic disparities in hospital utilization for childbirth. This can inform policymakers and health practitioners in improving maternal health in Indonesia
References
N. Madise, A. Nandi, B. Wong y S. Razvi, "Achieving Maternal and Neonatal Mortality Development Goals Effectively: A Cost-Benefit Analysis", J Benefit Cost Anal, vol. 14, no. S1, pp. 206-234, 2023, doi: 10.1017/bca.2023.24.
T. Alfvén, "Strengthened health systems and a multisectoral approach are needed to achieve sustainable health gains for children,"Acta Paediatrica, vol. 111, no. 11. Wiley Online Library, pp. 2054-2022, 2022. Wiley Online Library, pp. 2054-2055, 2022. doi: 10.1111/apa.16522.
J. A. Kavle, "Opportunities to Strengthen Women's Nutrition Within Maternal Health Service Delivery: Reflections From Global Health Implementation", Am J Public Health, vol. 112, no. S8, pp. S760-S762, 2022, doi: 10.2105/AJPH.2022.307026.
E. Fuentes-Afflick, J. M. Perrin, K. H. Moley, Á. Díaz, M. C. McCormick, y M. C. Lu, "Optimizing Health And Well-Being For Women And Children: Commentary highlights interventions and recommends key improvements in programs and policies to optimize health and well-being among women and children in the United States", Health Aff, vol. 40, nº 2, pp. 212-218, 2021, doi: 10.1377/hlthaff.2020.01504.
Rokom, "Turunkan Angka Kematian Ibu melalui Deteksi Dini dengan Pemenuhan USG di Puskesmas". Consultado: 03 de mayo de 2024. En línea]. Disponible: https://sehatnegeriku.kemkes.go.id/baca/rilis-media/20230115/4842206/turunkan-angka-kematian-ibu-melalui-deteksi-dini-dengan-pemenuhan-usg-di-puskesmas/
M. D. Anggraeni, R. Setiyani, E. Triyanto, A. Iskandar, D. Nani y A. Fatoni, "Exploring the antenatal care challenges faced during the COVID-19 pandemic in rural areas of Indonesia: a qualitative study", BMC Pregnancy Childbirth, vol. 23, nº 1, p. 179, 2023, doi: 10.1186/s12884-023-05495-8.
S. N. Jamil, E. N. Octavia, B. N. Fadliah y E. M. Gandirawati, "Factors Associated with the Use of Skilled Birth Attendants in Indonesia", International Journal of Clinical Inventions and Medical Sciences (IJCIMS), vol. 4, nº 2, pp. 49-55, 2022, doi: 10.36079/lamintang.ijcims-0402.407.
L. M. Ryan, M. A. Mahmood, I. Mufiddah, M. Yulianti y C. O. Laurence, "Concomitant illnesses in pregnancy in Indonesia: A health systems analysis at a District level", PLoS One, vol. 17, nº 12, p. e0279592, 2022, doi: 10.1371/journal.pone.0279592.
H. Herwansyah, K. Czabanowska, S. Kalaitzi y P. Schröder-Bäck, "Exploring the influence of sociodemographic characteristics on the utilization of maternal health services: a study on community health centers setting in province of Jambi, Indonesia", Int J Environ Res Public Health, vol. 19, nº 14, p. 8459, 2022, doi: 10.3390/ijerph19148459.
A. D. Laksono, R. D. Wulandari, N. Rohmah, R. Rukmini y T. Tumaji, "Regional disparities in hospital utilisation in Indonesia: a cross-sectional analysis data from the 2018 Indonesian Basic Health Survey", BMJ Open, vol. 13, n.º 1, p. e064532, 2023, doi: 10.1136/bmjopen-2022-064532.
R. D. Wulandari, A. D. Laksono, R. Mubasyiroh, R. Rachmalina, M. Ipa y N. Rohmah, "Hospital utilization among urban poor in Indonesia in 2018: is government-run insurance effective?", BMC Public Health, vol. 23, n.º 1, p. 92, 2023, doi: 10.1186/s12889-023-15017-y.
N. A. Damayanti, R. D. Wulandari e I. A. Ridlo, "Maternal health care utilization behavior, local wisdom, and associated factors among women in urban and rural areas, Indonesia", Int J Womens Health, pp. 665-677, 2023, doi: 10.2147/IJWH.S379749.
Á. L. Cáceres, R. M. Ramesh, P. Newmai, R. Kikon y A. Deckert, "Perceptions, health seeking behavior and utilization of maternal and newborn health services among an indigenous tribal community in Northeast India-a community-based mixed methods study", Front Public Health, vol. 11, p. 1139334, 2023, doi: 10.3389/fpubh.2023.1139334.
M. Bacciaglia, H. T. Neufeld, E. Neiterman, A. Krishnan, S. Johnston y K. Wright, "Indigenous maternal health and health services within Canada: a scoping review", BMC Pregnancy Childbirth, vol. 23, nº 1, p. 327, 2023, doi: 10.1186/s12884-023-05645-y.
J. T. Lee, B. McPake, L. P. Putri, K. Anindya, D. A. Puspandari y T. Marthias, "The effect of health insurance and socioeconomic status on women's choice in birth attendant and place of delivery across regions in Indonesia: a multinomial logit analysis", BMJ Glob Health, vol. 8, n.º 1, p. e007758, 2023, doi: 10.1136/bmjgh-2021-007758.
T. Marthias et al., "Associations between Indonesia's national health insurance, effective coverage in maternal health and neonatal mortality: a multilevel interrupted time-series analysis 2000-2017", J Epidemiol Community Health, vol. 76, nº 12, pp. 999-1010, 2022, doi: 10.1017/bca.2023.24.
D. A. Musadad, T. J. Angkasawati, Y. Usman, M. Kelly y C. Rao, "Implementation research for developing Civil Registration and Vital Statistics (CRVS) Systems: lessons from Indonesia", BMJ Glob Health, vol. 8, nº 7, p. e012358, 2023, doi: 10.1136/bmjgh-2023-012358.
F. M. Ekawati, M. Muchlis y A. Tuteja, "Adopting international recommendations to design a model for maternal health service to cope with pandemic disruption for Indonesian primary care", BMC Pregnancy Childbirth, vol. 23, nº 1, p. 132, 2023, doi: 10.1186/s12884-023-05433-8.
H. Chu y A. Rammohan, "Childhood immunization and age-appropriate vaccinations in Indonesia", BMC Public Health, vol. 22, nº 1, p. 2023, 2022, doi: 10.1186/s12889-022-14408-x.
L. M. Ryan, M. A. Mahmood, I. Mufiddah, M. Yulianti y C. O. Laurence, "Concomitant illnesses in pregnancy in Indonesia: A health systems analysis at a District level", PLoS One, vol. 17, nº 12, p. e0279592, 2022, doi: 10.1371/journal.pone.0279592.
F. Misu y K. Alam, "Comparison of inequality in utilization of postnatal care services between Bangladesh and Pakistan: Evidence from the Demographic and Health Survey 2017-2018", BMC Pregnancy Childbirth, vol. 23, n.º 1, p. 461, 2023, doi: 10.1186/s12884-023-05778-0.
S. S. A. Chowdhury, S. Kundu y A. Bin Sharif, "Socioeconomic and geographical inequalities in using skilled birth attendants during delivery in Bangladesh over two decades", BMC Pregnancy Childbirth, vol. 23, nº 1, p. 430, 2023, doi: 10.1186/s12884-023-05754-8.
C. B. Ngandu, D. Momberg, A. Magan, L. Chola, S. A. Norris, y R. Said-Mohamed, "The association between household socio-economic status, maternal socio-demographic characteristics and adverse birth and infant growth outcomes in sub-Saharan Africa: a systematic review,"J Dev Orig Health Dis, vol. 11, no. 4, pp. 317-334, 2020, doi: 10.1017/S2040174419000680.
F. Fasina, G. Oni, D. Azuh y A. Oduaran, "Impact of mothers' socio-demographic factors and antenatal clinic attendance on neonatal mortality in Nigeria", Cogent Soc Sci, vol. 6, nº 1, p. 1747328, ene. 2020, doi: 10.1080/23311886.2020.1747328.
D. M. Kangbai, D. A. Bandoh, A. Manu, J. Y. Kangbai, E. Kenu y A. Addo-Lartey, "Socio-economic determinants of maternal health care utilization in Kailahun District, Sierra Leone, 2020", BMC Pregnancy Childbirth, vol. 22, nº 1, p. 276, 2022, doi: 10.1186/s12884-022-04597-z.
A. Singh, A. Kumar y P. Pranjali, "Utilization of maternal healthcare among adolescent mothers in urban India: evidence from DLHS-3", PeerJ, vol. 2, p. e592, 2014, doi: 10.7717/peerj.592.
E. G. Henry et al., "The influence of quality maternity waiting homes on utilization of facilities for delivery in rural Zambia", Reprod Health, vol. 14, pp. 1-10, 2017, doi: doi.org/10.1186/s12978-017-0328-z.
S. Goli, Moradhvaj, A. Rammohan, Shruti y J. Pradhan, "High spending on maternity care in India: What are the factors explaining it?", PLoS One, vol. 11, n.º 6, p. e0156437, 2016, doi: 10.1371/journal.pone.0156437.
M. Tanou y Y. Kamiya, "Assessing the impact of geographical access to health facilities on maternal healthcare utilization: evidence from the Burkina Faso demographic and health survey 2010", BMC Public Health, vol. 19, pp. 1-8, 2019, doi: 10.1186/s12889-019-7150-1.
Y. Li et al., "Urban-sub-urban-rural variation in the supply and demand of emergency medical services", Front Public Health, vol. 10, p. 1064385, 2023, doi: 10.3389/fpubh.2022.1064385.
Z. Tao y M. Zhao, "Planning for equal transit-based accessibility of healthcare facilities: A case study of Shenzhen, China", Socioecon Plann Sci, vol. 88, p. 101666, 2023, doi: 10.1016/j.seps.2023.101666.
K. Chen et al., "Do hospital and rail accessibility have a consistent influence on housing prices? Empirical evidence from China", Front Environ Sci, vol. 10, p. 1044600, 2022, doi: 10.3389/fenvs.2022.1044600.
H. Fox, S. M. Topp, D. Lindsay y E. Callander, "Ethnic, socio-economic and geographic inequities in maternal health service coverage in Australia", Int J Health Plann Manage, vol. 36, nº 6, pp. 2182-2198, 2021, doi: 10.1002/hpm.3277.
Y. H. Gebresilassie y A. M. Teka, "What drives the ruralurban disparities in maternitycare services utilisation? Evidence from Ethiopia", F1000Res, vol. 12, p. 666, 2023, doi: 10.12688/f1000research.134166.1.
K. Z. Lwin y S. Punpuing, "Determinants of institutional maternity services utilization in Myanmar,"PLoS One, vol. 17, no. 4, p. e0266185, 2022, doi: 10.1371/journal.pone.0266185.
D. Amwonya, N. Kigosa y J. Kizza, "Female education and maternal health care utilization: evidence from Uganda", Reprod Health, vol. 19, nº 1, p. 142, 2022, doi: 10.1186/s12978-022-01432-8.
P. Singh, K. K. Singh y P. Singh, "Maternal health care service utilization among young married women in India, 1992-2016: trends and determinants", BMC Pregnancy Childbirth, vol. 21, pp. 1-13, 2021, doi: 10.1186/s12884-021-03607-w.
L. O. Ajah et al., "Choice of birth place among antenatal clinic attendees in rural mission hospitals in Ebonyi State, South-East Nigeria,"PLoS One, vol. 14, no. 11, p. e0211306, 2019, doi: 10.1371/journal.pone.0211306.
M. D. Huesch, E. Currid-Halkett, y J. N. Doctor, "Public hospital quality report awareness: evidence from National and Californian Internet searches and social media mentions, 2012,"BMJ Open, vol. 4, no. 3, p. e004417, 2014, doi: 10.1136/bmjopen-2013-004417.
R. Janakiraman, E. Park, E. M. Demirezen y S. Kumar, "The effects of health information exchange access on healthcare quality and efficiency: An empirical investigation", Manage Sci, vol. 69, nº 2, pp. 791-811, 2023, doi: 10.1287/mnsc.2022.4378.
H. Leino-Kilpi et al., "Knowledge received by hospital patients-a factor connected with the patient-centred quality of nursing care,"Int J Nurs Pract, vol. 21, no. 6, pp. 689-698, 2015, doi: 10.1111/ijn.12277.
D. Larrotta-Castillo, J. Moreno-Chaparro, A. Amaya-Moreno, H. Gaitán-Duarte, and K. Estrada-Orozco, "Health literacy interventions in the hospital setting: an overview,"Health Promot Int, vol. 38, no. 3, p. daac043, 2023, doi: 10.1093/heapro/daac043.
R. Patel, S. P. Marbaniang, S. Srivastava, P. Kumar y S. Chauhan, "Why women choose to deliver at home in India: a study of prevalence, factors, and socio-economic inequality", BMC Public Health, vol. 21, nº 1, p. 1785, 2021, doi: 10.1186/s12889-021-11779-5.
P. Paul y P. Chouhan, "Socio-demographic factors influencing utilization of maternal health care services in India", Clin Epidemiol Glob Health, vol. 8, no. 3, pp. 666-670, 2020, doi: 10.1016/j.cegh.2019.12.023.
E. Atake, "Socio-economic inequality in maternal health care utilization in Sub-Saharan Africa: Evidence from Togo", Int J Health Plann Manage, vol. 36, nº 2, pp. 288-301, 2021, doi: 10.1002/hpm.3083.
C. Okoli, M. Hajizadeh, M. M. Rahman y R. Khanam, "Geographical and socioeconomic inequalities in the utilization of maternal healthcare services in Nigeria: 2003-2017", BMC Health Serv Res, vol. 20, pp. 1-14, 2020, doi: 10.1186/s12913-020-05700-w.
L. Adler y J. Azuri, "Maternal perinatal depression and health services utilisation in the first 2 years of life: a cohort study", BMJ Open, vol. 11, nº 11, p. e052873, 2021, doi: 10.1136/bmjopen-2021-052873.
A. Banke-Thomas et al., "A mixed-methods study of maternal health care utilisation in six referral hospitals in four sub-Saharan African countries before and during the COVID-19 pandemic", BMJ Glob Health, vol. 7, nº 2, p. e008064, 2022, doi: 10.1136/bmjgh-2021-008064.
A. A. Creanga et al., "Maternal health policy environment and the relationship with service utilization in low-and middle-income countries", J Glob Health, vol. 13, 2023, doi: 10.7189/jogh.13.04025.
N. Gauld, S. Martin, O. Sinclair, H. Petousis-Harris, F. Dumble y C. C. Grant, "Influences on pregnant women's and health care professionals' behaviour regarding maternal vaccination: a qualitative interview study", Vaccines (Basilea), vol. 10, n.º 1, p. 76, 2022, doi: 10.3390/vaccines10010076.
T. Mekonnen, T. Dune, y J. Perz, "Maternal health service utilisation of adolescent women in sub-Saharan Africa: a systematic scoping review", BMC Pregnancy Childbirth, vol. 19, pp. 1-16, 2019, doi: 10.1186/s12884-019-2501-6.
D. T. Stein, M. F. Rakhmadi, A. Dutta y J. I. Ugaz, "Attributes of funding flows and quality of maternal health services in a mixed provider payment system: A cross-sectional survey of 108 healthcare providers in Indonesia", World Med Health Policy, vol. 15, nº 2, pp. 179-193, 2023, doi: 10.1002/wmh3.545.
S. Balla, M. I. K. Sk, M. Ambade y B. Hossain, "Distress financing in coping with out-of-pocket expenditure for maternity care in India", BMC Health Serv Res, vol. 22, nº 1, p. 288, 2022, doi: 10.1186/s12913-022-07656-5.
H. Fox, S. M. Topp, E. Callander y D. Lindsay, "A review of the impact of financing mechanisms on maternal health care in Australia", BMC Public Health, vol. 19, pp. 1-14, 2019, doi: 10.1186/s12889-019-7850-6.
M. L. Dennis, L. Benova, T. Abuya, M. Quartagno, B. Bellows y O. M. R. Campbell, "Initiation and continuity of maternal healthcare: examining the role of vouchers and user-fee removal on maternal health service use in Kenya", Health Policy Plan, vol. 34, n.º 2, pp. 120-131, 2019, doi: Initiation and continuity of maternal healthcare: examining the role of vouchers and user-fee removal on maternal health service use in Kenya.
T. A. Gebremedhin, I. Mohanty y T. Niyonsenga, "Public health insurance and maternal health care utilization in India: Evidence from the 2005-2012 mothers' cohort data", BMC Pregnancy Childbirth, vol. 22, nº 1, p. 155, 2022, doi: 10.1186/s12884-022-04441-4.
L. P. O. Were, E. Were, R. Wamai, J. Hogan y O. Galarraga, "The Association of Health Insurance with institutional delivery and access to skilled birth attendants: evidence from the Kenya demographic and health survey 2008-09", BMC Health Serv Res, vol. 17, pp. 1-10, 2017, doi: 10.1186/s12889-019-7850-6.
Downloads
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.